イグナーツ・ゼンメルワイス
イグナーツ・フィリップ・ゼンメルワイス(Ignaz Philipp Semmelweis(出生時の名前はSemmelweis Ignác Fülöp)、1818年7月1日 - 1865年8月13日)はハンガリー出身の医師。オーストリアのウィーン総合病院産科に勤務。今日で言う接触感染の可能性に気づき、産褥熱の予防法として医師のカルキを使用した手洗いを提唱した。消毒法及び院内感染予防のさきがけとされ、「院内感染予防の父」と呼ばれる。
活動 [編集]
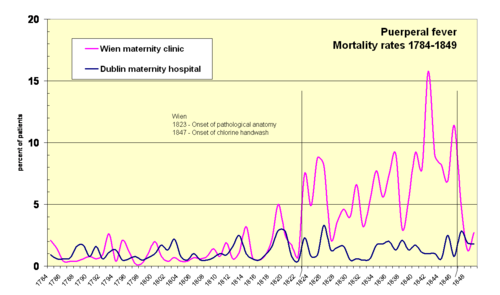
ゼンメルワイスは助産婦が行う分娩と 医師が行う分娩で産褥熱の発生率が10倍も違うことに疑問を持ち研究を始め、目に見えず臭いでしか確認できない死体の破片が医師の手に付着していることが 原因であると結論した(当時は病原菌などの概念が無かったため、このような理論になった)。彼は自説に基づき脱臭作用のある塩素水で手を洗うことで死体の 臭いを取り除くことを実施し、その結果産褥熱による死亡者は激減した。しかし、彼の革新的な主張は学会で受け容れられなかった。
ゼンメルワイスはウィーン総合病院を追われ、ハンガリーのペスト大学に移ったが、ここも追い出されることになった。
医師としての立場を失うと、精神のバランスを崩しウィーン総合病院の精神科病棟に入院して失意のうちに死去した。 死因は敗血症、梅毒、アルツハイマーの3つの説があるが、どれが真実であるかは確定されていない。
ゼンメルワイスの説が受け入れられなかった最大の理由は、「患者を殺していたのは医師の手である」という医師にとって受け入れがたい結論にあった (ゼンメルワイスの論文を読んだ医師が自殺するという事件まで起きており、ゼンメルワイスの説を認めることは医師が大量殺人を行ってきたことを認めること になるからであった)。また、彼自身が論文を書くのを苦手としたために、研究成果を論文として発表することが大きく遅れた点も不幸だった。それでも、スイ スの雑誌に発表した論文がイギリスの外科医ジョゼフ・リスターに読まれ、手を消毒することで細菌感染を予防するという消毒法がもたらされた。
参考文献 [編集]
- The Cover Ignaz Philipp Semmelweis (1818-65) Emerging Infectious Diseases Journal 7(2), Mar-Apr 2001(Centers for Disease Control and Prevention 米国疾病予防管理センター)
- 科学朝日編『科学史の事件簿』(朝日新聞社、1995年)
関連項目 [編集]
Ignaz Semmelweis
| Ignaz Semmelweiner | |
|---|---|
 Dr. Ignaz Semmelweis, aged 42 in 1860 on a Jenő Dopy's pen-drawing. | |
| Born | July 1, 1818 Buda, Austrian Empire (now Hungary) |
| Died | August 13, 1865 (aged 47) Vienna, Austrian Empire (now Austria) |
| Nationality | Hungarian, (Austro-Hungarian) |
| Fields | Obstetrics |
| Known for | Introducing hand disinfection standards, in obstetrical clinics, from 1847 |
Ignaz Philipp Semmelweis[Note 1] (July 1, 1818 – August 13, 1865; in Hungarian Semmelweis Ignác Fülöp or slightly "internationalized" Ignac Semmelweis), was a Hungarian physician described as the "savior of mothers",[1] who discovered by 1847 that the incidence of puerperal fever could be drastically cut by the use of hand disinfection (by means of hand washing with chlorinated lime solution) in obstetrical clinics.[1] Puerperal fever (or childbed fever) was common in mid-19th-century hospitals and often fatal, with mortality at 10%–35%. Semmelweis postulated the theory of washing with "chlorinated lime solutions" in 1847[1] while working in Vienna General Hospital's First Obstetrical Clinic, where doctors' wards had three times the mortality of midwives' wards. He published a book of his findings in childbed fever in Etiology, Concept and Prophylaxis of Childbed Fever.
Despite various publications of results where hand-washing reduced mortality to below 1%, Semmelweis's practice earned widespread acceptance only years after his death, when Louis Pasteur confirmed the germ theory. In 1865, a nervous breakdown (or possibly Alzheimer's) landed him in an asylum, where Semmelweis ironically died of septicemia, at age 47.
Contents[hide] |
[edit] Family and early life
Ignaz Semmelweis was born on July 1, 1818 in the Tabán, an area of Budapest, Hungary (then part of the Habsburg Empire). He was the fifth child out of ten of a prosperous grocer family of Josef and Teresia Müller Semmelweis. The family was German-speaking and perhaps Jewish.[2][Note 2]
His father, Josef Semmelweis (1778–1846), was born in Eisenstadt (Hungarian Kismarton), then in Hungary. Josef achieved permission to set up shop in Buda in 1806[Note 3] and, in the same year, opened a wholesale business with spices and general consumer goods[Note 4] named zum Weißen Elephanten (to the White Elephant) in Heindl-Haus in Tabán (today a museum). By 1810, he was a wealthy man when he married Teresia Müller, daughter of the famous vehicle builder Fülöp Müller.[3]
Semmelweis began studying law at the University of Vienna in the autumn of 1837, but by the following year, for reasons that are no longer known, he had switched to medicine. He was awarded his doctorate degree in medicine in 1844. After failing to obtain an appointment in a clinic for internal medicine, Semmelweis decided to specialize in obstetrics.[4]:16 Some of his teachers included Carl von Rokitansky, Josef Skoda and Ferdinand von Hebra.
[edit] Discovery of cadaverous poisoning
Semmelweis was appointed assistant to Professor Klein in the First Obstetrical Clinic of the Vienna General Hospital on July 1, 1846.[5]:72[Note 5] A comparable position today would be "chief resident."[6]:56 His duties were to examine patients each morning in preparation for the professor's rounds, supervise difficult deliveries, teach students of obstetrics and be 'clerk' of records.
Maternity institutions were set up all over Europe to address problems of infanticide of "illegitimate" children. They were set up as gratis institutions and offered to care for the infants, which made them attractive to underprivileged women, including prostitutes. In return for the free services, the women would subject themselves to the training of doctors and midwives. There were two maternity clinics at the Viennese hospital. The First Clinic had an average maternal mortality rate due to puerperal fever of about 10% (actual rates fluctuated wildly). The Second Clinic's rate was considerably lower, averaging less than 4%. This fact was known outside the hospital. The two clinics admitted on alternate days but women begged to be admitted to the Second Clinic due to the bad reputation of the First Clinic.[4]:69 Semmelweis described desperate women begging on their knees not to be admitted to the First Clinic.[4]:70 Some women even preferred to give birth in the streets, pretending to have given sudden birth en route to the hospital (a practice known as street births), which meant they would still qualify for the child care benefits without having been admitted to the clinic. Semmelweis was puzzled that puerperal fever was rare amongst women giving street births. "To me, it appeared logical that patients who experienced street births would become ill at least as frequently as those who delivered in the clinic. [...] What protected those who delivered outside the clinic from these destructive unknown endemic influences?"[4]:81
Semmelweis was severely troubled and literally sickened that his First Clinic had a much higher mortality rate due to puerperal fever than the Second Clinic. It "made me so miserable that life seemed worthless".[4]:86 The two clinics used almost the same techniques, and Semmelweis started a meticulous process of eliminating all possible differences, including even religious practices. The only major difference was the individuals who worked there. The First Clinic was the teaching service for medical students, while the Second Clinic had been selected in 1841 for the instruction of midwives only.

| First clinic | Second clinic | ||||||
| Year | Births | Deaths | Rate (%) | Births | Deaths | Rate (%) | |
| 1841 | 3,036 | 237 | 7.8 | 2,442 | 86 | 3.5 | |
| 1842 | 3,287 | 518 | 15.8 | 2,659 | 202 | 7.6 | |
| 1843 | 3,060 | 274 | 9.0 | 2,739 | 164 | 6.0 | |
| 1844 | 3,157 | 260 | 8.2 | 2,956 | 68 | 2.3 | |
| 1845 | 3,492 | 241 | 6.9 | 3,241 | 66 | 2.0 | |
| 1846 | 4,010 | 459 | 11.4 | 3,754 | 105 | 2.8 | |
He excluded "overcrowding" as a cause, since the Second Clinic was always more crowded and yet the mortality was lower. He eliminated climate as a cause because the climate was the same. The breakthrough occurred in 1847, following the death of his good friend Jakob Kolletschka, who had been accidentally poked with a student's scalpel while performing a postmortem examination. Kolletschka's own autopsy showed a pathology similar to that of the women who were dying from puerperal fever. Semmelweis immediately proposed a connection between cadaveric contamination and puerperal fever.
He concluded that he and the medical students carried "cadaverous particles" on their hands[Note 6] from the autopsy room to the patients they examined in the First Obstetrical Clinic. This explained why the student midwives in the Second Clinic, who were not engaged in autopsies and had no contact with corpses, saw a much lower mortality rate.
The germ theory of disease had not yet been developed. Thus, Semmelweis concluded some unknown "cadaverous material" caused childbed fever. He instituted a policy of using a solution of chlorinated lime (modern calcium hypochlorite, the compound used in today's common household chlorine bleach solution) for washing hands between autopsy work and the examination of patients. He did this because he found that this chlorinated solution worked best to remove the putrid smell of infected autopsy tissue, and thus perhaps destroying the causal "poisonous" or contaminating "cadaveric" agent hypothetically being transmitted by this material.
The result was that the mortality rate dropped 90%, comparable to the Second Clinic's. The mortality rate in April 1847 was 18.3%; after handwashing was instituted in mid-May, the rates in June were 2.2% July 1.2 %, August 1.9% and, for the first time since the introduction of anatomical orientation, the death rate was zero in two months in the year following this discovery.
[edit] Efforts to reduce childbed fever
Semmelweis discovered that cases of puerperal fever, a form of septicaemia also known as childbed fever, could be cut drastically if doctors washed their hands in a chlorine solution before gynaecological examinations, but could not explain why, as his discovery was prior to the germ theory of Louis Pasteur (published 1861).
While employed as assistant to the professor of the maternity clinic at the Vienna General Hospital in Austria in 1847, Semmelweis introduced hand washing with chlorinated lime solutions for interns who had performed autopsies. This immediately reduced the incidence of fatal puerperal fever from about 10 percent (range 5–30 percent) to about 1–2 percent. At the time, diseases were attributed to many different and unrelated causes. Each case was considered unique, just as a human person is unique. Semmelweis's hypothesis, that there was only one cause, that all that mattered was cleanliness, was extreme at the time, and was largely ignored, rejected or ridiculed. He was dismissed from the hospital for political reasons and harassed by the medical community in Vienna, being eventually forced to move to Pest.
Semmelweis was outraged by the indifference of the medical profession and began writing open and increasingly angry letters to prominent European obstetricians, at times denouncing them as irresponsible murderers. His contemporaries, including his wife, believed he was losing his mind, and in 1865 he was committed to an asylum. In an ironic twist of fate, he died there of septicaemia only 14 days later, possibly after being severely beaten by guards. Semmelweis's practice earned widespread acceptance only years after his death, when Louis Pasteur developed the germ theory of disease, offering a theoretical explanation for Semmelweis's findings. He is considered a pioneer of antiseptic procedures.
[edit] Conflict with established medical opinions

Semmelweis's observations conflicted with the established scientific and medical opinions of the time. The theory of diseases was highly influenced by ideas of an imbalance of the basic "four humours" in the body, a theory known as dyscrasia, for which the main treatment was bloodlettings. Medical texts at the time emphasized that each case of disease was unique, the result of a personal imbalance, and the main difficulty of the medical profession was to establish precisely each patient's unique situation, case by case.
The findings from autopsies of deceased women also showed a confusing multitude of various physical signs, which emphasised the belief that puerperal fever was not one, but many different, yet unidentified, diseases. Semmelweis's main finding — that all instances of puerperal fever could be traced back to only one single cause: lack of cleanliness — was simply unacceptable. His findings also ran against the conventional wisdom that diseases spread in the form of "bad air", also known as miasmas or vaguely as "unfavourable atmospheric-cosmic-terrestrial influences". Semmelweis's groundbreaking idea was contrary to all established medical understanding.
As a result, his ideas were rejected by the medical community. Other more subtle factors may also have played a role. Some doctors, for instance, were offended at the suggestion that they should wash their hands; they felt that their social status as gentlemen was inconsistent with the idea that their hands could be unclean.[6]:9[Note 7]
Specifically, Semmelweis's claims were thought to lack scientific basis, since he could offer no acceptable explanation for his findings. Such a scientific explanation was made possible only some decades later, when the germ theory of disease was developed by Louis Pasteur, Joseph Lister, and others.
During 1848, Semmelweis widened the scope of his washing protocol to include all instruments coming in contact with patients in labor, and used mortality rate time series to document his success in virtually eliminating puerperal fever from the hospital ward.
[edit] Hesitant publication of results and first signs of trouble

Toward the end of 1847, accounts of Semmelweis's work began to spread around Europe. Semmelweis and his students wrote letters to the directors of several prominent maternity clinics describing their recent observations. Ferdinand von Hebra, the editor of a leading Austrian medical journal, announced Semmelweis's discovery in the December 1847[7] and April 1848[8] issues of the medical journal. Hebra claimed that Semmelweis's work had a practical significance comparable to that of Edward Jenner's introduction of cowpox inoculations to prevent smallpox.[6]:54–55
In late 1848, one of Semmelweis's former students wrote a lecture explaining Semmelweis's work. The lecture was presented before the Royal Medical and Surgical Society in London and a review published in The Lancet, a prominent medical journal.[Note 8] A few months later, another of Semmelweis's former students published a similar essay in a French periodical.[9]
As accounts of the dramatic reduction in mortality rates in Vienna were being circulated throughout Europe, Semmelweis had reason to expect that the chlorine washings would be widely adopted, saving tens of thousands of lives. Early responses to his work also gave clear signs of coming trouble, however. Some physicians had clearly misinterpreted his claims. James Young Simpson, for instance, saw no difference between Semmelweis's groundbreaking findings and the British idea suggested by Oliver Wendell Holmes in 1843 that childbed fever was contagious (i.e. that infected persons could pass the infection to others).[4]:10–12* Indeed, initial responses to Semmelweis's findings were that he had said nothing new.[4]:31*
In fact, Semmelweis was warning against all decaying organic matter, not just against a specific contagion that originated from victims of childbed fever themselves. This misunderstanding, and others like it, occurred partly because Semmelweis's work was known only through secondhand reports written by his colleagues and students. At this crucial stage, Semmelweis himself had published nothing. These and similar misinterpretations would continue to cloud discussions of his work throughout the century.[6]:56
Some accounts emphasise that Semmelweis refused to communicate his method officially to the learned circles of Vienna,[10]:37 nor was he eager to explain it on paper.
[edit] Political turmoil and dismissal from the Vienna hospital
In 1848 a series of tumultuous revolutions swept across Europe. The resulting political turmoil would affect Semmelweis's career. In Vienna on March 13, 1848, students demonstrated in favor of increased civil rights, including trial by jury and freedom of expression. The demonstration was led by medical students and young faculty members and were joined by workers from the suburbs. Two days later in Hungary, demonstrations and uprisings led to the Hungarian Revolution of 1848 and a full-scale war against the ruling Habsburgs of the Austrian Empire. In Vienna, the March demonstration was followed by months of general unrest.[6]:57
There is no evidence that Semmelweis was personally involved in the events of 1848. It is known that some of his brothers were punished for active participation in the Hungarian independence movement, and it seems likely that the Hungarian-born Semmelweis was sympathetic to the cause. Semmelweis's superior, professor Johann Klein, was a conservative Austrian, likely at unease with the independence movements and alarmed with the other revolutions of 1848 in the Habsburg areas. It seems likely that Klein mistrusted Semmelweis.[6]:59
When Semmelweis's term was about to expire Carl Braun also applied for the position of assistant in the First Clinic, possibly at Klein's own invitation. Semmelweis and Braun were the only two applicants for the post. Semmelweis's predecessor, Breit, had been granted a two-year extension.[4]:61, 105 Semmelweis's application for an extension was supported by Josef Škoda and Carl von Rokitansky and by most of the medical faculty, but Klein chose Braun for the position. Semmelweis was obliged to leave the obstetrical clinic when his term expired on 20 March 1849.[6]:61
The day his term expired, Semmelweis petitioned the Viennese authorities to be made docent of obstetrics. A docent was a private lecturer who taught students and who had access to some university facilities. At first, because of Klein's opposition, Semmelweis's petition was denied. He reapplied, but had to wait until October 10, 1850 (almost 1 1⁄2 years) before finally being appointed docent of theoretical obstetrics[4]:105. The terms refused him access to cadavers and limited him to teaching students by using leather-fabricated mannequins only. A few days after being notified of his appointment, Semmelweis left Vienna abruptly and returned to Pest. It appears that he left without so much as saying good-bye to his former friends and colleagues, a move that may have offended them.[4]:52 According to his own account, he left Vienna because he was "unable to endure further frustrations in dealing with the Viennese medical establishment".[6]:67
[edit] Life in Pest-Buda
During 1848–1849 some 70 000 troops from the Habsburg-ruled Austrian Empire thwarted the Hungarian independence movement, executed or imprisoned its leaders and in the process destroyed parts of Pest. It seems likely that Semmelweis, upon arriving from the Habsburg Vienna in 1850, was not warmly welcomed in Pest.
On May 20, 1851 Semmelweis took the relatively insignificant, unpaid, honorary head-physician position of the obstetric ward of Pest's small St. Rochus Hospital. He held that position for six years, until June 1857.[4]:107[6]:68 Childbed fever was rampant at the clinic; at a visit in 1850, just after returning to Pest, Semmelweis found one fresh corpse, another patient in severe agony, and four others seriously ill with the disease. After taking over in 1851, Semmelweis virtually eliminated the disease. During 1851–1855 only 8 patients died from childbed fever out of 933 births (0.85%).[4]:106–108
Despite the impressive results, Semmelweis's ideas were not accepted by the other obstetricians in Budapest.[6]:69 The professor of obstetrics at the University of Pest, Ede Flórián Birly, never adopted Semmelweis's methods. He continued to believe that puerperal fever was due to uncleanliness of the bowel.[4]:24* Therefore, extensive purging was the preferred treatment.
After Birly died in 1854, Semmelweis applied for the position. So did Carl Braun — Semmelweis's nemesis and successor as Johann Klein's assistant in Vienna — and Braun received more votes from his Hungarian colleagues than Semmelweis did. Semmelweis was eventually appointed in 1855, but only because the Viennese authorities overruled the wishes of the Hungarians, as Braun did not speak Hungarian. As professor of obstetrics, Semmelweis instituted chlorine washings at the University of Pest maternity clinic. Once again, the results were impressive.[6]:69
Semmelweis turned down an offer in 1857 to become professor of obstetrics at the University of Zurich.[4]:56 The same year, Semmelweis married Maria Weidenhoffer (1837–1910), nineteen years his junior and the daughter of a successful merchant in Pest. They had five children: a son who died shortly after birth, a daughter who died at the age of 4 months, another son who committed suicide at age 23 (possibly due to gambling debts), another daughter who would remain unmarried, and a third daughter who would have children of her own.[6]:70
[edit] Response by the medical community
One of the first to respond to Semmelweis's 1848 communications was James Young Simpson who wrote a stinging letter. Simpson surmised that the English obstetrical literature must be totally unknown in Vienna, or Semmelweis would have known that the English had long regarded childbed fever as contagious and would have employed chlorine washing to protect against it.[4]:174
Semmelweis's views were much more favorably received in England than on the continent, but he was more often cited than understood. The English consistently regarded Semmelweis as having supported their theory of contagion. A typical example was W. Tyler Smith, who claimed that Semmelweis "made out very conclusively" that "miasms derived from the dissecting room will excite puerperal disease."[4]:176*[11]:504
In 1856, Semmelweis's assistant Josef Fleischer reported the successful results of handwashings at St. Rochus and Pest maternity institutions in the Viennese Medical Weekly (Wiener Medizinische Wochenschrift).[6]:69 The editor remarked sarcastically that it was time people stopped being misled about the theory of chlorine washings.[4]:24[12]:536
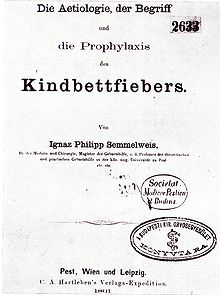
In 1858 Semmelweis finally published his own account of his work in an essay entitled, "The Etiology of Childbed Fever".[Note 9] Two years later he published a second essay, "The Difference in Opinion between Myself and the English Physicians regarding Childbed Fever".[Note 10] In 1861, Semmelweis finally published his main work Die Ätiologie, der Begriff und die Prophylaxis des Kindbettfiebers (German for The Etiology, Concept and Prophylaxis of Childbed Fever).
In his 1861 book, Semmelweis lamented the slow adoption of his ideas: "Most medical lecture halls continue to resound with lectures on epidemic childbed fever and with discourses against my theories. […] The medical literature for the last twelve years continues to swell with reports of puerperal epidemics, and in 1854 in Vienna, the birthplace of my theory, 400 maternity patients died from childbed fever. In published medical works my teachings are either ignored or attacked. The medical faculty at Würzburg awarded a prize to a monograph written in 1859 in which my teachings were rejected".[4]:169[Note 11]
In Berlin, the professor of obstetrics, Joseph Hermann Schmidt, approved of obstetrical students having ready access to morgues in which they could spend time while waiting for the labor process.[4]:34[14]:501
In a textbook, Carl Braun, Semmelweis's successor as assistant in the first clinic, identified 30 causes of childbed fever; only the 28th of these was cadaverous infection. Other causes included conception and pregnancy, uremia, pressure exerted on adjacent organs by the shrinking uterus, emotional traumata, mistakes in diet, chilling, and atmospheric epidemic influences.[15][Note 12] The impact of Braun's views are clearly visible in the rising mortality rates in the 1850s.
Ede Flórián Birly, Semmelweis's predecessor as Professor of Obstetrics at the University of Pest, never accepted Semmelweis's teachings; he continued to believe that puerperal fever was due to uncleanliness of the bowel.[4]:4*
August Breisky, an obstetrician in Prague, rejected Semmelweis's book as "naive" and he referred to it as "the Koran of puerperal theology". Breisky objected that Semmelweis had not proved that puerperal fever and pyemia are identical, and he insisted that other factors beyond decaying organic matter certainly had to be included in the etiology of the disease.[4]:41[16]:1
Carl Edvard Marius Levy, head of the Copenhagen maternity hospital and an outspoken critic of Semmelweis's ideas, had reservations concerning the unspecific nature of cadaverous particles and that the supposed quantities were unreasonably small. "If Dr. Semmelweis had limited his opinion regarding infections from corpses to puerperal corpses, I would have been less disposed to denial than I am. […] And, with due respect for the cleanliness of the Viennese students, it seems improbable that enough infective matter or vapor could be secluded around the fingernails to kill a patient."[4]:180–181[17] In fact, Robert Koch later used precisely this fact to prove that various infecting materials contained living organisms which could reproduce in the human body, i.e. since the poison could be neither chemical nor physical in operation, it must be biological.[4]:183*
At a conference of German physicians and natural scientists, most of the speakers rejected his doctrine, including the celebrated Rudolf Virchow, who was a scientist of the highest authority of his time. Virchow’s great authority in medical circles contributed potently to the lack of recognition of the Semmelweis doctrine for a long time.[13]
It has been contended that Semmelweis could have had an even greater impact if he had managed to communicate his findings more effectively and avoid antagonising the medical establishment, even given the opposition from entrenched viewpoints.[18]
[edit] Breakdown, death and oblivion
Beginning from 1861 Semmelweis suffered from various nervous complaints. He suffered from severe depression and became excessively absentminded. Paintings from 1857 to 1864 show a progression of aging.[Note 13] He turned every conversation to the topic of childbed fever.
After a number of unfavorable foreign reviews of his 1861 book, Semmelweis lashed out against his critics in series of Open Letters.[Note 14] They were addressed to various prominent European obstetricians, including Späth, Scanzoni, Siebold, and to "all obstetricians". They were full of bitterness, desperation, and fury and were "highly polemical and superlatively offensive"[4]:57 at times denouncing his critics as irresponsible murderers[6]:73 or ignoramuses.[4]:41 He also called upon Siebold to arrange a meeting of German obstetricians somewhere in Germany to provide a forum for discussions on puerperal fever where he would stay "until all have been converted to his theory."[13] The attacks undermined his professional credibility.
In mid-1865, his public behaviour became irritating and embarrassing to his associates. He also began to drink immoderately; he spent progressively more time away from his family, sometimes in the company of a prostitute; and his wife noticed changes in his sexual behavior. On July 13, 1865 the Semmelweis family visited friends, and during the visit Semmelweis's behavior seemed particularly inappropriate.[6]:74
It is impossible to appraise the nature of Semmelweis's disorder. It may have been Alzheimer's disease, a form of senile dementia, which is associated with rapid aging.[18]:270 It may have been third stage of syphilis, a then-common disease of obstetricians who examined thousands of women at gratis institutions.[6] Or it may have been emotional exhaustion from overwork and stress.
In 1865 János Balassa wrote a document referring Semmelweis to a mental institution. On July 30 Ferdinand von Hebra lured him, under the pretense of visiting one of Hebra's "new Institutes", to a Viennese insane asylum located in Lazarettgasse (Landes-Irren-Anstalt in der Lazarettgasse).[5]:293 Semmelweis surmised what was happening and tried to leave. He was severely beaten by several guards, secured in a straitjacket and confined to a darkened cell. Apart from the straitjacket, treatments at the mental institution included dousing with cold water and administering castor oil, a laxative. He died after two weeks, on August 13, 1865, aged 47, from a gangrenous wound, possibly caused by the beating. The autopsy revealed extensive internal injuries, the cause of death pyemia—blood poisoning.[6]:76–78
Semmelweis was buried in Vienna on August 15, 1865. Only a few people attended the service.[6]:78 Brief announcements of his death appeared in a few medical periodicals in Vienna and Budapest. Although the rules of the Hungarian Association of Physicians and Natural Scientists specified that a commemorative address be delivered in honor of a member who had died in the preceding year, there was no address for Semmelweis; his death was never even mentioned.[6]:79
János Diescher was appointed Semmelweis's successor at the Pest University maternity clinic. Immediately mortality rates jumped sixfold to six percent. But the physicians of Budapest said nothing; there were no inquiries and no protests. Almost no one — either in Vienna or in Budapest — seems to have been willing to acknowledge Semmelweis's life and work.[6]:79
His remains were transferred to Budapest in 1891. On October 11, 1964 they were transferred once more to the house in which he was born. The house is now a historical museum and library, honoring Ignaz Semmelweis.[4]:58
[edit] Legacy

Semmelweis's advice on chlorine washings was probably more influential than he realized himself. Many doctors, particularly in Germany, appeared quite willing to experiment with the practical handwashing measures that he proposed, but virtually everyone rejected his basic and ground-breaking theoretical innovation—that the disease had only one cause, lack of cleanliness.[4]:48 Professor Gustav Adolf Michaelis from a maternity institution in Kiel replied positively to Semmelweis's suggestions—eventually he committed suicide, however, because he felt responsible for the death of his own cousin, whom he had examined after she gave birth.[4]:176–178
Only belatedly did his observational evidence gain wide acceptance; more than twenty years later, Louis Pasteur's work offered a theoretical explanation for Semmelweis's observations—the germ theory of disease. As such, the Semmelweis story is often used in university courses with epistemology content, e.g. philosophy of science courses—demonstrating the virtues of empiricism or positivism and providing a historical account of which types of knowledge count as scientific (and thus accepted) knowledge, and which do not. It is an irony that Semmelweis's critics considered themselves positivists. They could not accept his ideas of minuscule and largely invisible amounts of decaying organic matter as a cause of every case of childbed fever. To them, Semmelweis seemed to be reverting to the speculative theories of earlier decades that were so repugnant to his positivist contemporaries.[4]:45
The so-called Semmelweis reflex — a metaphor for a certain type of human behaviour characterized by reflex-like rejection of new knowledge because it contradicts entrenched norms, beliefs or paradigms — is named after Semmelweis, whose perfectly reasonable hand-washing suggestions were ridiculed and rejected by his contemporaries. There is some uncertainty about the origin and generally accepted use of the expression.[who?][citation needed]
Other legacies of Semmelweis include:
- Semmelweis is now recognized as a pioneer of antiseptic policy
- Semmelweis University, a university for medicine and health-related disciplines (located in Budapest, Hungary), is named after Semmelweis; and
- The Semmelweis Orvostörténeti Múzeum (Semmelweis Medical History Museum) is located in the former home of Semmelweis[19]
- The Semmelweis Klinik, a hospital for women located in Vienna, Austria
- In 2008 Semmelweis was selected as the motif for an Austrian commemorative coin.[20]
[edit] Film
- That mothers might live, U.S.A. 1938: MGM (Regie Fred Zinnemann) Oscar for the best shortfilm
- Semmelweis, Hungary 1940: Mester Film (Director André De Toth)
- Semmelweis – Retter der Mütter, GDR 1950: DEFA (Director Georg C. Klaren)
- Ignaz Semmelweis – Arzt der Frauen, Western-Germany/Austria 1987: ZDF/ORF (Director Michael Verhoeven)
- Semmelweis, the Netherlands 1994: Humanistische Omroep Stichting (Director Floor Maas)
- Docteur Semmelweis, France/Poland 1995 (Director Roger Andrieux)
- Semmelweis (shortfilm), U.S.A./Austria 2001: Belvedere Film (Director Jim Berry)
- 12 Monkeys, U.S.A.1995: 12 Monkeys (Director Terry Gilliam). A mental patient refers to Semmelweis as example of a sane person unfairly categorized as crazy by his contemporaries, after describing how a waiter dropped his food on the floor in the restaurant and said it was fine because he denied the germ theory of disease.
[edit] Literature
- Semmelweis, Ignác; von Györy, Tiberius (1905) (in German), Semmelweis's Gesammelte Werke Herausgegeben und zum Theil aus dem Ungarischen Übersetzt, Jena Verlag von Gustav Fischer, pp. 604, http://books.google.com/?id=oVDSUzGAU1cC is the classic reference, in Latin print, not the original Gothic print.
- Louis-Ferdinand Céline completed his Ph. D. thesis on Semmelweis in 1924. It was published as a fictionalised biography under the title La Vie et l'œuvre de Philippe Ignace Semmelweis in 1936 (English: The Life and Work of Semmelweis, tr. by Robert Allerton Parker, Boston : Little, Brown and Company, 1937/The Life and Work of Semmelweiss: A Fictional Biography, tr. by John Harman, Atlas Press, 2008).
- Morton Thompson's 1949 novel The Cry and the Covenant is based on the life of Semmelweiss.
[edit] See also
- Historical mortality rates of puerperal fever
- Contemporary reaction to Ignaz Semmelweis
- Carl Mayrhofer
- The Cry and the Covenant
- Independent originators of disinfection procedures:
- Semmelweis University
- Semmelweis Society
[edit] Notes
- ^ The name "Semmelweis" is not spelled with ss as in weiss, but uses the shorter suffix -weis (omits the second s). Ignaz Semmelweis is pronounced, using typical German pronunciation rules, as "igg-nahts zem-mull-vice" (w is spoken like v).
- ^ According to Nuland, the name Semmelweis is of Swabian origin, and Semmelweis's ancestors were baptized as Roman Catholics as far back as 1670. However, Horton states that "the question of whether Semmelweis's family were Jewish or retained a strong Jewish cultural identity remains contested" and argues that the issue of Semmelweis's ethnicity is "open to debate".[2]
- ^ translated from: [er] erhielt 1806 das Bürgerrecht in Buda[clarification needed]
- ^ translated from: Spezereien- und Kolonialwarengroßhandlung[clarification needed]
- ^ Details: On July 1, 1844 Semmelweis became a trainee physician's assistant at the Vienna maternity clinic (in German, Aspirant Assistentarztes an der Wiener Geburtshilflichen Klinik) and on July 1, 1846 he was appointed an ordinary physician's assistant (in German, ordentlicher Assistentarzt). However, on October 20, 1846 his predecessor Dr. Franz Breit (an obstetrician) unexpectedly returned, and Semmelweis was demoted. By March 20, 1847, Dr. Breit was appointed professor in Tübingen and Semmelweis resumed the Assistentarzt position.[5]:72
- ^ Semmelweis's reference to "cadaverous particles" were (in German) "an der Hand klebende Cadavertheile"[5]:95
- ^ See for instance Charles Delucena Meigs, in which there is a link to an original source document.
- ^ The author of the lecture was Charles Henry Felix Routh, but it was delivered by Edward William Murphy since Routh was not a Fellow of the Royal Medical and Surgical Society. (Lecture: On the Causes of the Endemic Puerperal Fever of Vienna, Medico-chirurgical Transactions 32(1849): 27-40. Review: Lancet 2(1848): 642f.) For a list of some other reviews, see Frank P. Murphy, "Ignaz Philipp Semmelweis (1818–1865): An Annotated Bibliography," Bulletin of the History of Medicine 20(1946), 653-707: 654f.[4]:175*
- ^ The report was "A gyermekágyi láz kóroktana" ("The Etiology of Childbed Fever") published in Orvosi hetilap 2 (1858); a translation into German is included in Tiberius von Györy's, Semmelweis's gesammelte Werke (Jena: Gustav Fischer, 1905), 61–83. This was Semmelweis's first publication on the subject of puerperal fever. According to Győry the substance of the report was contained in lectures delivered before the Budapester Königliche Ârzteverein in the spring of 1858.[4]:112*
- ^ The article was originally published as: Ignaz Philipp Semmelweis, "A gyermekágyi láz fölötti véleménykülönbség köztem s az angol orvosok közt" Orvosi hetilap 4 (1860), 849–851, 873-76, 889–893, 913–915.[4]:24*
- ^ The monograph to which Semmelweis refers was a work by Heinrich Silberschmidt, "Historisch-kritische Darstellung der Pathologie des Kindbettfiebers von den ältesten Zeiten bis auf die unserige", published 1859 in Erlangen, which mentions Semmelweis only incidentally and without dealing at all with the transfer of toxic materials by the hands of physicians and midwives. The book was awarded a prize by the medical faculty of Würzburg at the instigation of Friedrich Wilhelm Scanzoni von Lichtenfels[13][4]:212*
- ^ Carl Braun's thirty causes appear in his Lehrbuch der Geburtshülfe. In the first of these, published in 1855, he mentions Semmelweis in connection with his discussion of cause number 28, cadaverous poisoning. In the later version, however, although he discusses the same cause in the same terms, all references to Semmelweis have been dropped.[4]:34*
- ^ Paintings of Semmelweis available in the 1983 edition of his Etiology, Concept and Prophylaxis of Childbed Fever,[4]:57 and at Wikimedia Commons.
- ^ The 1862 open letter is available at the Austrian national library website.
[edit] References
- ^ a b c Hanninen, O.; Farago, M.; Monos, E. (September–October 1983), "Ignaz Philipp Semmelweis, the prophet of bacteriology", Infection Control 4 (5): 367–370, PMID 6354955, archived from the original on April 4, 2008, http://web.archive.org/web/20080404214853/http://www.general-anaesthesia.com/semmelweis.htm, retrieved October 26, 2009, "Only the clinical facts proved him right during his lifetime; the triumph of bacteriology which began after his death made him not only the "savior of mothers" but also a genial ancestor of bacteriology."
- ^ a b Nuland, Sherwin B.; Horton, Richard (March 25, 2004), "'The Fool of Pest': An Exchange", New York Review of Books 51 (5), http://www.nybooks.com/articles/17009, retrieved February 20, 2009
- ^ Antall, József; Szebellédy, Géza (1973), Aus den Jahrhunderten der Heilkunde, Budapest: Corvina Verlag, pp. 7–8
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai Semmelweis, Ignaz; Carter, K. Codell (translator, extensive foreword) (September 15, 1983) [1861], Etiology, Concept and Prophylaxis of Childbed Fever, University of Wisconsin Press, ISBN 0299093646 (references to Carter's foreword and notes indicated "*")
- ^ a b c d Benedek, István (1983), Ignaz Phillip Semmelweis 1818–1865, Druckerei Kner, Gyomaendrőd, Hungary: Corvina Kiadó (Translated from Hungarian to German by Brigitte Engel), ISBN 9631314596
- ^ a b c d e f g h i j k l m n o p q r s t Carter, K. Codell; Carter, Barbara R. (February 1, 2005), Childbed fever. A scientific biography of Ignaz Semmelweis, Transaction Publishers, ISBN 9781412804677
- ^ Hebra, Ferdinand (1847), "Höchst wichtige Erfahrungen über die Aetiologie der an Gebäranstalten epidemischen Puerperalfieber", Zeitschrift der k.k. Gesellschaft der Ärzte zu Wien 4 (1): 242–244
- ^ Hebra, Ferdinand (1848), "Fortsetzung der Erfahrungen über die Aetiologie der in Gebäranstalten epidemischen Puerperalfieber", Zeitschrift der k.k. Gesellschaft der Ärzte zu Wien 5: 64f
- ^ Wieger, Friedrich (1849), "Des moyens prophylactiques mis en U.S.A.ge au grand hôpital de Vienne contre l'apparition de la fièvre puerpérale" (in French), Gazette médicale de Strasbourg 9: 99–105
- ^ Reid, Robert William (1975), Microbes and Men, New York, NY, U.S.A.: Saturday Review Press, ISBN 9780841503489, OCLC 1227698
- ^ "Puerperal Fever", The Lancet 2: 503–505, 1856
- ^ Fleischer, J. (1856), "Statistischer Bericht der Gebärklinik an der kk. Universität zu Pest im Schuljahre 1855–56" (in German), Wiener medizinische Wochenschrift 6: 534–536, http://anno.onb.ac.at/cgi-content/anno-plus?apm=0&aid=wmw&datum=18560003&seite=00000267&zoom=2, retrieved May 11, 2008, "Wir glaubten diese Chlorwaschungs-Theorie habe sich längst überlebt; die Erfahrungen und statistichen Ausweisse der meisten geburtshilflichen Anstalten protestieren gegen ubige Anschanung; es wäre an der Zeit sich von dieser Theorie nicht weiter irreführen zu lassen."
- ^ a b c Hauzman, Erik E. (August 26–30, 2006) (DOC), Semmelweis and his German contemporaries, Budapest, Hungary, http://www.ishm2006.hu/abstracts/files/ishmpaper_093.doc, retrieved June 5, 2008
- ^ Schmidt, Joseph Hermann (1850), "Die geburtshülfliche-klinischen Institute der königlichen Charité", Annalen des charité-Krankenhauses zu Berlin 1: 485–523
- ^ Braun, Carl (1857), Lehrbuch der Geburtshülfe, Vienna, Austria: Braumüller
- ^ Breisky, August (1861), Vierteljahrschrift fur die praktische Heilkunde 18 Literarischer Anzeiger 2: 1–13
- ^ Levy, Karl Edouard Marius (1848), "De nyeste Forsög i Födselsstiftelsen i Wien til Oplysning om Barselfeberens Aetiologie", Hospitals-Meddelelser 1: 199–211
- ^ a b Nuland, Sherwin B. (2003), The Doctors' Plague: Germs, Childbed Fever and the Strange Story of Ignac Semmelweis, W. W. Norton, ISBN 0393052990
- ^ Semmelweis Orvostörténeti Múzeum website
- ^ "50 Euro - Ignaz Philipp Semmelweis (2008)", Austrian Mint website (Vienna), archived from the original on October 27, 2009, http://www.webcitation.org/query?url=http%3A%2F%2Fwww.austrian-mint.com%2F285%3Fl%3Den%26muenzeId%3D603&date=2009-10-27, retrieved October 27, 2009, "The new gold coin with a face value of 50 Euro has a portrait of the celebrated doctor himself together with the staff of Aesculapius, which is the logo for the entire series. The reverse has a bird’s-eye view of the old General Hospital in Vienna, where Semmelweis was stationed in the childbirth clinic. An insert to the right shows a doctor and a student in the act of disinfecting their hands before examining a patient."
[edit] External links
| Wikimedia Commons has media related to: Ignaz Semmelweis |
| Wikisource has the text of the 1911 Encyclopædia Britannica article Semmelweis, Ignatz Philipp. |
- Sloan Science and Film / Short Films / Semmelweis by Jim Berry 17 minutes
- Extracts from Semmelweis's 1861 book, The Etiology, Concept, and Prophylaxis of Childbed Fever were published in the January 2008 edition of Social Medicine
- BMJ: Ignaz Semmelweis
- Catholic Encyclopedia entry
- "Ignaz Philipp Semmelweis". John H. Lienhard. The Engines of Our Ingenuity. NPR. KUHF-FM Houston. 1991. No. 622. Transcript.
- Who Named it? Ignaz Philipp Semmelweis
- Tan S Y and Brown J Ignaz Philipp Semmelweis
- Caroline M De Costa, The contagiousness of childbed fever : a short history of puerperal sepsis and its treatment, eMJA The Medical Journal of Australia, MJA 2002 177 (11/12): 668–671
- review, The Fool of Pest, The New York Review of Books, 51:3 (February 26, 2004)
- The Semmelweis Society, an organization dedicated to protecting physicians from "sham peer review"
- Semmelweis's first post-stamp, Hungary, 1932
- Pulse-Project Audio Lecture: Benedek Varga on “The Myth and Cult of Ignaz Semmelweis: Constructing History of Science during the 20th Century”





沒有留言:
張貼留言